Focusing foreign aid on infectious diseases has allowed a rise in cancer and diabetes that African governments don’t have resources to fight, says Dr Githinji Gitahi
Health services in Africa are at risk of “collapse in the next few years” due to soaring chronic diseases, a senior public health leader has warned.

Foreign aid to Africa has been focused on infectious diseases, leaving conditions such as cancer and diabetes to escalate, said Dr Githinji Gitahi, group CEO of Amref Health Africa.
In sub-Saharan Africa, non-communicable diseases (NCDs), including hypertension, diabetes and heart disease accounted for 37% of deaths in 2019, up from 24% in 2000. They are forecast to become the leading cause of death in the region by 2030 – driven by factors such as unhealthy western-style diets, less active lifestyles and air pollution.
“Aid is not charity” and will inevitably follow donor countries’ own interests such as stopping infectious diseases that could spread overseas, said Gitahi, who called for Africa’s leaders to step up their own work on controlling NCDs.
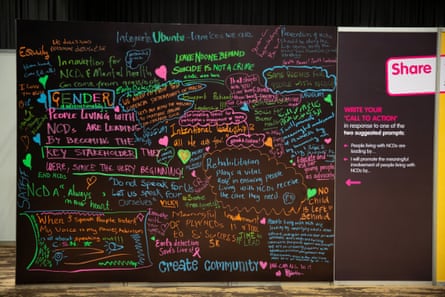
Gitahi spoke to the Guardian at the Global NCD Alliance Forum in Kigali, Rwanda, earlier this month, a gathering of more than 700 delegates from 89 countries.

The challenge is vast, according to Gitahi. “Africa has a big risk of collapse of health systems in the next few years because of NCDs […] 50% of all admissions in a typical African hospital are NCDs, yet 80% of NCD care is out of pocket. And governments don’t have money to actually take care of NCDs.”
The blame lies with multinational corporations chasing profits, he said, and with governments failing to bring in regulations to put a brake on their activities. “Politicians think about the next election,” he said. “This issue is about the next generation.”
Gitahi, from Kenya, said global health and foreign aid spending had historically focused on diseases that could affect the donors themselves. Less than 3% of development spending for health goes to NCDs.
“That is why there is so much focus on TB, HIV, because when you keep HIV low in Kenya, you keep it out of your country because people travel, and people carry diseases,” he said. “But for cancer, for hypertension, for diabetes … that’s non-infectious.

“The people who should care about that are their governments because [NCDs] are taking away people from active social and economic participation. Because the governments don’t have enough money […] it is likely to continue being a neglected problem.”
The forum’s delegates were meeting as a result of decisions by the US administration to freeze much of its overseas aid spending and to issue stop work orders to current programmes. Amref’s work has been affected, Gitahi said.
“We do about $250m [£197m] of work a year […] about $50m of that is actually US government partnerships,” he said, in areas including maternal and child health, HIV work and laboratory and health system strengthening.
Some Amref staff have been placed on unpaid leave, Gitahi said, though he was optimistic that some of the work will restart after the 90-day review period announced by Donald Trump’s officials.
“We hope that at the end of it, they will continue with programming, as they say, that’s aligned to their foreign policy, but actually protects communities and community lives and protects Americans themselves,” Gitahi said. “I keep saying aid is not charity. Aid is strategic investment by a country to protect its own internal interests. That’s what it has always been.”
African governments will need to become more efficient and to tackle corruption, he suggested, and to embrace taxation of unhealthy goods, such as tobacco, alcohol and sugar, with the proceeds earmarked for health programmes. They will also need to work on the prevention of ill health, Gitahi said, suggesting they “copy and paste” regulations from western countries that ban things such as the advertising of foods high in sugar, salt or fat to children.
US funding accounts for half of all development assistance in Africa, he said, or $6.5bn out of $13bn. African governments will not be able to completely replace lost funding, Gitahi said, because their economies are not large enough. It may mean reframing goals to provide universal health care to cover “100% of the poor” rather than the entire population.
“Africa cannot raise enough money from its fiscal space, from its GDP, to actually take care of all social services,” he said. “Africa needs solidarity.”
In the end, the international community should see that solidarity was important for global security, he said. “When you have a weak health system in any country, it is like having an insecure airspace in any country. That [poses] a risk to the entire world.”
Source: The Guardian



















